There may not be a safe off-ramp for some taking GLP-1 drugs, study suggests
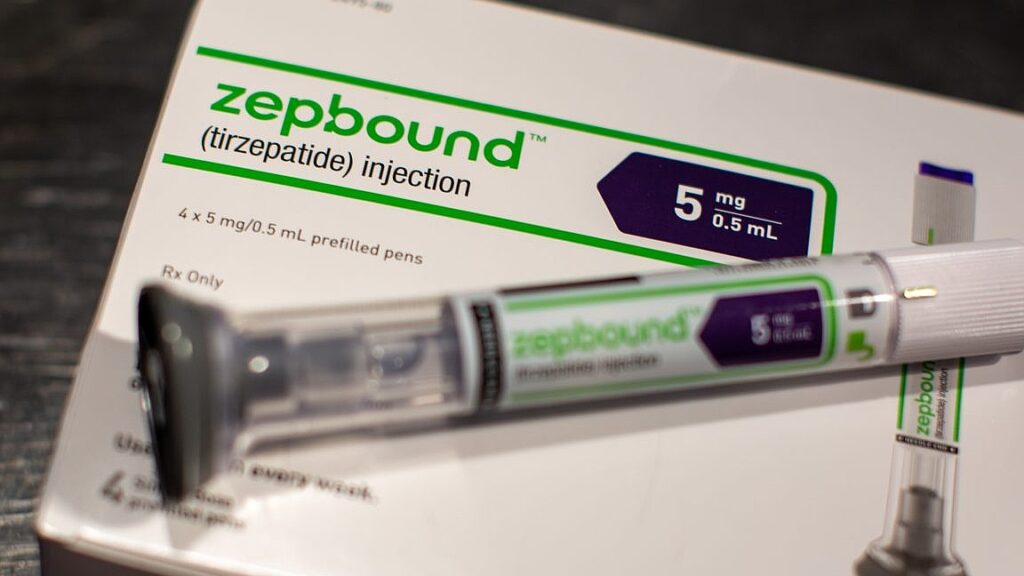
The rising popularity of GLP-1 weight-loss medications, such as tirzepatide (Zepbound), has made a significant impact on obesity rates across the United States. Recent findings published in JAMA Internal Medicine reveal that while these medications can lead to substantial weight loss and improvements in cardiovascular and metabolic health, the long-term sustainability of these benefits remains uncertain. In a clinical trial, participants who stopped taking tirzepatide not only regained much of the weight they had lost but also experienced a concerning reversal of health improvements. Key metrics such as blood pressure, cholesterol levels, hemoglobin A1c, and fasting insulin all reverted to pre-treatment levels, raising questions about the long-term efficacy and safety of discontinuing these medications.
In light of these findings, experts from the University of Pittsburgh, Elizabeth Oczypok and Timothy Anderson, propose a shift in how we view these medications. They suggest rebranding them from “weight loss” drugs to “weight management” drugs, emphasizing the potential necessity for lifelong use to maintain health benefits. This perspective highlights an important consideration for both patients and healthcare providers: while GLP-1 medications can be effective in achieving weight loss and improving metabolic health, a comprehensive strategy for long-term weight management and health maintenance is crucial. As the medical community grapples with these challenges, the conversation around obesity treatment continues to evolve, signaling a need for further research and innovative solutions in the fight against obesity.
The popularity of GLP-1 weight-loss medications continues to soar—and their uptake is helping to push down obesity rates on a national scale—but a safe, evidence-based way off the drugs isn’t yet in clear view.
An
analysis published this week in JAMA Internal Medicine
found that most participants in a clinical trial who were assigned to stop taking tirzepatide (Zepbound from Eli Lilly) not only regained significant amounts of the weight they had lost on the drug, but they also saw their cardiovascular and metabolic improvements slip away. Their blood pressure went back up, as did their cholesterol, hemoglobin A
1c
(used to assess glucose control levels), and fasting insulin.
In
an accompanying editorial
, two medical experts at the University of Pittsburgh, Elizabeth Oczypok and Timothy Anderson, suggest that this new class of drugs should be rebranded from “weight loss” drugs to “weight management” drugs, which people may need to take indefinitely.
Read full article
Comments