How Medicaid’s New Work Requirement Will Work
In a significant shift in the landscape of healthcare access for low-income Americans, recent changes in federal policy are poised to create new hurdles for enrollment in Medicaid and other assistance programs. As the U.S. government moves to unwind pandemic-era protections that allowed for continuous enrollment in these programs, millions of individuals who relied on these safety nets are now at risk of losing their coverage. The end of the public health emergency has prompted states to reassess their Medicaid rolls, leading to a complex and often daunting re-enrollment process that many low-income families may find challenging to navigate.
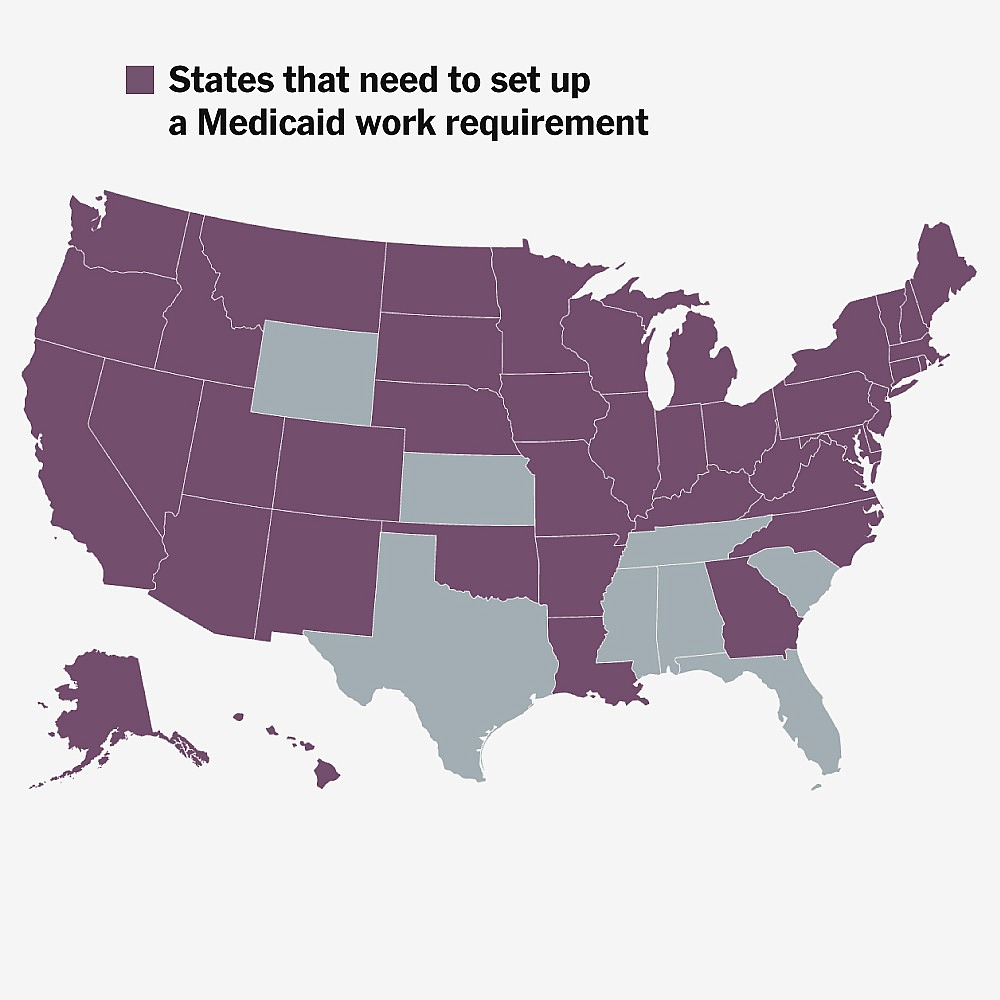
Historically, the continuous enrollment policy helped maintain stability for vulnerable populations during the COVID-19 pandemic, but as states begin to conduct eligibility reviews, they are faced with the daunting task of building new bureaucratic systems to manage the influx of applications and renewals. Many states, particularly those with limited resources, are struggling to handle the anticipated surge in workload. For instance, states like Texas and Florida, which have large populations of uninsured individuals, are likely to see significant increases in demand for assistance as families attempt to re-enroll. The complexities of the new regulations, combined with the varying levels of state preparedness, could lead to confusion and delays, ultimately exacerbating the difficulties faced by low-income Americans in accessing essential healthcare services.
The implications of these changes are profound. Without proper guidance and support, many eligible individuals may fall through the cracks, leading to increased rates of uninsured populations. This situation is particularly concerning given the ongoing challenges posed by rising healthcare costs and the lingering effects of the pandemic on public health. Advocacy groups are calling for immediate action to streamline the re-enrollment processes and ensure that outreach efforts effectively reach those most in need. As states grapple with these new responsibilities, the importance of robust support systems and clear communication becomes increasingly critical to safeguard the health and well-being of millions of Americans.
Poor Americans will face new challenges to enroll, and states will have to build new bureaucracies.